Perhaps one of the most common states of unconsciousness you might be familiar with is the coma state. Coma is a state of unconsciousness from which a person cannot be roused. A person in the coma state is neither awake nor aware. He’s alive but incapable of responding to stimuli.
You may be able to wake a sleeping person up by shaking them or talking loudly but this won’t work for a person who’s in a coma.
People usually slip into a coma when they experience a severe head injury that may cause the brain to move back and forth in the skull, thereby tearing blood vessels and nerve fibres.
This tearing causes the brain tissue to swell which presses down on blood vessels, blocking the flow of blood (and hence, oxygen) to the brain.
It’s this lack of oxygen supply to the brain that damages the brain tissues and results in a loss of consciousness that manifests as a coma.
Coma may also be caused by other conditions such as aneurysm and ischemic stroke, which also block oxygen supply to the brain. Encephalitis, meningitis, low and high blood sugar levels can also lead to coma.
Degrees or levels of unconsciousness
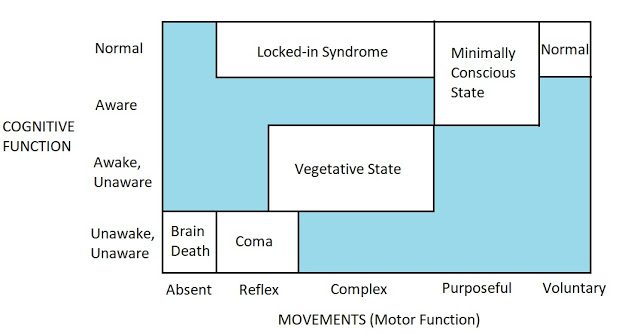
How deeply a person falls into unconsciousness depends on the severity of the injury or illness. Coma belongs to a family of disorders called disorders of consciousness that represent different degrees of unconsciousness.
To understand these types of unconsciousness states let’s say Jack suffered a head injury during an accident.
If Jack’s brain completely ceases to function, doctors say that he’s brain dead. It means he has permanently lost consciousness and the ability to breathe.
If Jack slips into a coma, the brain doesn’t shut down fully but works at a minimal level. He may or may not be capable of breathing but he can’t respond to any stimuli (such as pain or sound). He cannot perform any voluntary actions. His eyes remain closed and there’s a lack of sleep-wake cycle in the coma state.
Say, after a few weeks of staying in the coma, Jack shows signs of recovery. He’s now able to open his eyes, blink, sleep, wake, and yawn. He may also be able to move his limbs, grimace, and make chewing movements whilst still being incapable of responding to stimuli. This state is known as the vegetative state.
Instead of slipping into the vegetative state, Jack may slip into what is known as the minimally conscious state. In this state, Jack can show non-reflexive and purposeful behaviours but is unable to communicate. He is intermittently aware.
If Jack is aware and awake, can wake and sleep, and even communicate with eyes but is unable to do voluntary actions (partially or completely) then he’s in a locked-in state. He’s sort of locked-in in his body.1
General anesthesia given to patients renders them temporarily unconscious so that major operations and surgeries, that can otherwise be very painful, can be performed. General anesthesia can be thought of as an artificially induced reversible coma.2
Recovery from coma
A coma usually lasts for only a few weeks and a person is able to recover gradually, transitioning from unconsciousness to consciousness. Brain stimulation via therapy and exercises can aid the process of recovery.
Presumably, the brain circuits need stimulation and activation to restore their normal function.
In fact, a study showed that coma patients who heard familiar stories repeated by family members recovered consciousness significantly faster and had an improved recovery than those who didn’t hear any such stories.3
The longer a person stays in a coma, the less the chances of recovery but there exist cases of people recovering from coma even after 10 years and 19 years.
Why people enter states of unconsciousness
A safety fuse in an electronic appliance melts and breaks the circuit if too much current passes through the circuit. This way the appliance and the circuit are protected from damage.
Injury-induced coma works in pretty much the same way, except that the brain isn’t entirely shut down (as in brain death) but operates at a minimal level.
When a severe internal injury is detected by your brain, it throws you into a coma state so that any further discretionary movement is avoided, blood loss is minimized, and the body’s resources are mobilized toward repair of an immediate threat to life.4
In this sense, coma is very similar to threat-induced fainting. While fainting is a response to a potential threat, coma is a response to an actual threat. While fainting prevents you from being injured, coma is your mind’s last attempt to save you when you’re actually injured.
References
- Mikolajewska, E., & Mikolajewski, D. (2012). Consciousness disorders as the possible effect of brainstem activity failure-Computational approach. Journal of Health Sciences, 2(2), 007-018.
- Brown, E. N., Lydic, R., & Schiff, N. D. (2010). General anesthesia, sleep, and coma. New England Journal of Medicine, 363(27), 2638-2650.
- Northwestern University. (2015, January 22). Family voices, stories speed coma recovery. ScienceDaily. Retrieved April 8, 2018 from www.sciencedaily.com/releases/2015/01/150122133213.htm
- Buss, D. (2015). Evolutionary psychology: The new science of the mind. Psychology Press.
